Introduction
Neurofibromatosis type 1 (NF1) is a heritable disorder involving the central and peripheral nervous system, the skin and soft tissue (neurocutaneous syndrome). The syndrome was also called in the past von Recklinghausen’s disease, a term that is no longer recommended by the WHO classification of genetic tumor syndromes [1–3].
Vascular disorders in the setting of NF1 are termed as NF1 vasculopathy. It includes arterial stenoses, aneurysms, dissections, arteriovenous malformations, vascular compression or invasion by neural tumors and spontaneous arterial rupture [1]. They occur at a rate of 0.4% to 6.4% in NF1 patients with most clinical symptoms emerging in the 5th decade of life [1, 4]. Although every artery may be affected, lesions in medium and large arteries predominate with rare aortic involvement [5]. Herein, we present the rare case of a 55-year-old male with NF1 who presented with abdominal aortic rupture and was treated urgently by endovascular abdominal aortic aneurysm repair (EVAR). Additionally, we present a literature review not only with similar cases of abdominal aortic ruptures but with all the aortic and iliac pathology in NF 1. We focus on the type of the vascular lesion, method of repair and outcome. Open repair (OR) and endovascular treatment (ET) each have their own advantages and disadvantages and currently there is uncertainty about which modality is superior. Although endovascular treatment is not suggested in connective tissue disorders, it is currently used in NF1 aortic rupture with acceptable results. While NF1-associated vasculopathy most commonly presents as renal artery stenosis, mid-aortic syndrome, and intracranial aneurysms, spontaneous avulsion of visceral arteries is exceedingly rare. This case adds to the limited number of reports describing NF1-related mesenteric and aortic complications, underlining the need for increased awareness of such unpredictable vascular events.
Case presentation
A 55-year-old male was transferred from a local hospital because of a 3-day persisting and worsening bilateral groin pain along with ultrasound findings of the periaortic mass and fluid. The pain started after lifting a heavy object. He was tachycardic (heart rate: 102 beats per minute) and normotensive (systolic blood pressure: 120 mm Hg), while innumerable neurofibromas and typical café-au-lait spots were noted throughout his face, trunk and upper extremities (Figure 1). His past medical history included arterial hypertension, dyslipidemia and NF1 diagnosed in childhood. He was an active smoker (25 pack years) and he discontinued his medicine (torasemide 2.5 mg o.d., olmesartan medoxomil 20 + 5 mg o.d. and rosuvastatin 10 mg o.d.) 6 months before admission. He had unspecified surgery for a carotid aneurysm 22 years ago. Computed tomography angiography (CTA) revealed an aortic rupture with gross extravasation of contrast media, 3.7 cm below the renal arteries, leading to a pseudoaneurysm and a large retroperitoneal hematoma (Figure 2). The abdominal aorta was locally ectatic near the rupture site and above the bifurcation; the right common iliac artery (CIA) was 3 cm in diameter (Figures 2, 3). It was obvious that aortic rupture was due to spontaneous avulsion of the inferior mesenteric artery (IMA) (Figure 4). The ascending thoracic aorta was 4 cm in diameter. We proceeded to ET due to concerns for open repair regarding the congenital vascular wall friability and the decreased morbidity and mortality associated with EVAR in ruptured abdominal aortic aneurysms (AAAs) [6]. Anticoagulation was achieved with 2500 units of heparin. A bifurcated endograft (Gore Excluder Conformable Endoprosthesis, W. L. Gore & Associates Inc., Flagstaff, Arizona, USA) was employed through both common femoral arteries cut down and placed infrarenally, after coil embolization of the right internal iliac artery (IIA). The right leg was landed in the external iliac artery (EIA), while the left placed in the CIA. No friability was noted in the common femoral arteries. Carotid duplex ultrasound was normal although the internal carotid artery (ICA) was narrow (2.5 mm in diameter). Brain magnetic resonance angiography revealed chronic obstruction of the petrous part of the ICA. Holter rhythm examination was positive for premature ventricular contractions. He was discharged on the 5th postoperative day (p.d.) in good condition. Follow-up CTA was performed on the 4th p.d., 1st month and 1st year after the operation depicting normal postoperative findings (Figure 5). The ethics committee approval and informed consent have been obtained. This case report was approved by the Institutional Review Board of the University Hospital of Patras (IRB no. 29/11-07-2018).
Figure 1
Multiple neurofibromas were noted throughout the patient’s face (A), trunk (B) and upper extremities. Typical café-au-lait spots were also present (C – red arrowheads: spots at the medial aspect of his right upper arm)

Figure 2
Computed tomography angiography (CTA) revealed an aortic rupture with gross extravasation of contrast media, 3.7 cm below the renal arteries, leading to a pseudoaneurysm and a large retroperitoneal hematoma (A – MPR reconstruction, sagittal view: red lightning bolt: aortic rupture, yellow arrows: aortic pseudoaneurysm, green arow: right common iliac artery aneurysm, B – Axial view: red lightning bolt: aortic rupture, yellow arrows: aortic pseudoaneurysm, light green arrowheads: focal aortic dilatation, light blue arrows: large retroperitoneal hematoma)
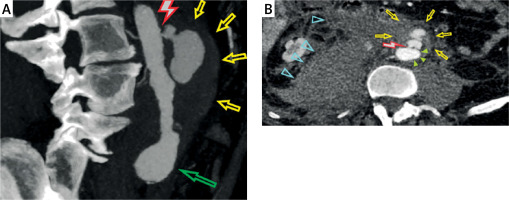
Figure 3
Computed tomography angiography (CTA), MPR reconstruction, coronal view (A – light green arrowheads: focal aortic dilatation near the rupture site, orange arrowheads: focal aortic dilatation above the aortic bifurcation), (B – red lightning bolt: aortic rupture, red lightning bolt: aortic rupture, light green arrowheads: focal aortic dilatation near the rupture site, orange arrowheads: focal aortic dilatation above the aortic bifurcation, light blue arrow: inferior mesenteric artery, green arow: right common iliac artery aneurysm)
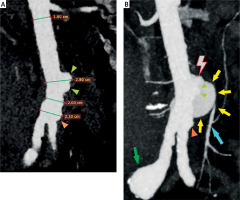
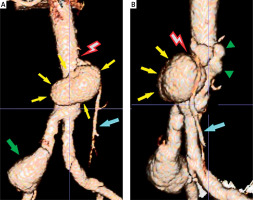
Figure 4
Computed tomography angiography (CTA), 3D-reconstruction (A – coronal view: red lightning bolt: aortic rupture due to avulsion of the inferior mesenteric artery, yellow arrows: aortic pseudoaneurysm, green arrow: right common iliac artery aneurysm, light blue arrow: inferior mesenteric artery), (B – oblique view: red lightning bolt: aortic rupture due to avulsion of the inferior mesenteric artery, yellow arrows: aortic pseudoaneurysm, green arrowheads: focal aortic dilatation, light blue arrow: inferior mesenteric artery)
Discussion
Clinical presentation of NF1
Neurofibromatosis type 1 is a rare congenital disorder with an autosomal dominant inheritance. It occurs in 1 of 3,000 births and is the most common subtype of neurofibromatosis. It is caused by genetic defects in the NF1 gene, which impairs the production of neurofibromin. This leads to alterations in connective and nerve tissue structure with various resulting phenotypes [3, 6, 7]. Clinical signs of NF1 may include café au lait macules, neurofibromas, axillary and inguinal freckling, Lisch nodules (iris hamartomas), skeletal abnormalities in 30–50% (kyphoscoliosis, sphenoid dysplasia or thinning of the long bone cortex, bone cysts, erosions of the bone surface), brain tumors and learning disabilities) [3, 8, 9]. Multiple lobulated neural tumors develop at the nerve trunks in the skin and the internal organs, and their locally destructive effects can be life-threatening [10, 11]. Neurofibromas are classified as localized (nodular type), diffuse or plexiform and can present as cutaneous, intraneural, or deep soft tissue lesions [10]. Cutaneous neurofibromas are benign tumors without potential for malignant transformation. Multiple paraspinal neurofibromas may arise from the spinal nerve roots [3, 10, 11]. Unlike peripherally located neurofibromas the paraspinal tumors more frequently undergo transformation into malignant peripheral nerve sheath tumors (MPNSTs) [10, 12]. Plexiform neurofibromas may cause extensive infiltration into surrounding tissues and may transform into MPNSTs in 8% to 16%. Compression of the gastro-intestinal, urinary, or pulmonary tracts by visceral neurofibromas may generate serious complications [3, 11, 13]. NF1 patients have a 34-fold increased risk for developing malignancies, including breast cancer [13, 14].
Clinical presentation of NF1 vasculopathy
Mutations in the NF1 gene result in loss of neurofibromin function, leading to dysregulated Ras/MAPK signaling. This contributes to endothelial dysfunction, vascular smooth muscle instability, and ultimately arterial fragility, increasing the risk of aneurysm formation and spontaneous rupture. NF1 vasculopathy includes arterial stenoses, aneurysms, dissections, arteriovenous malformations, intra-neurofibromatous hemorrhage and spontaneous arterial rupture, presenting in 0.4% to 6.4% [3, 10]. On the contrary, vascular lesions are extremely uncommon in neurofibromatosis type 2 (NF 2), which is characterized by the occurrence of acoustic schwannomas, meningiomas and gliomas, among other lesions [1]. Vascular lesions develop either by proliferation of nerves within the vessel walls (spindle cell proliferation) or from pressure necrosis of the arterial wall by external compression and/or invasion by nerve sheath tumors [3, 4, 15]. Consequently, vessels become fragile and vulnerable as in other connective tissue disorders, like Marfan’s and Ehlers Danlos syndrome, where the pathologic structure of the extracellular matrix may cause multiple aortic aneurysms, aortic dissection or rupture [16, 17]. NF1 lesions may appear in any artery of the body, but they have a predisposition for medium and large arteries. Consequently, they are seen more often in the renal, mesenteric, carotid, vertebral, intracranial, subclavian, innominate, coronary, peripheral arteries and the aorta [13, 14].
NF1 vasculopathy is usually asymptomatic, even in affliction of multiple vessels [8, 11]. There is a potential underappreciation of its occurrence because of the silent nature and the poor accessibility of most vascular lesions to the clinical examination. Indeed, according to an autopsy series of NF1 patients dying of other causes, vascular abnormalities were reported in 44% of them [8]. An English literature review from 1957 to 2005, reported 237 patients with NF1 [5]. Renal artery lesions with resulting renovascular hypertension were the most common finding (41%) [5, 8]. The carotid, vertebral and cerebral artery lesions were observed in 19% of patients, affecting mostly women (72%). The mean age was 38 years, varying between 22 and 54 years [10]. Veins may be also affected and spontaneous bleeding from internal jugular vein (IJV) has been reported [18, 19]. Additionally, pressure necrosis of the inferior vena cava (IVC) by a retroperitoneal neurofibroma leading to fatal retroperitoneal hemorrhage has been reported [20]. On the other hand, obstruction of the IVC by neurofibromas with a successful open repair is recorded in the literature [21]. The presence of pheochromocytomas can increase the risk of vascular rupture due to catecholamine-induced hypertension [22]. Cardiac involvement has been encountered in up to 27% of patients with NF1 with half of them having pulmonary artery stenosis [1].
Abdominal aortic coarctation or aneurysms, with or without renal and mesenteric involvement, are present in about 12% [5]. Spontaneous hemothoraces, retroperitoneal hematomas, subcutaneous and cerebral hematomas have been reported [6, 10]. Abdominal aorta involvement may be in the form of coarctation, aneurysm, acute dissection or rupture [23]. Coarctation is defined as a localized narrowing of the aortic lumen, most commonly near the ductus arteriosus. The middle aortic syndrome (MAS) is characterized by progressive narrowing of the abdominal aorta, associated with arterial hypertension and renal failure in children and young adults. It is typically compensated by the development of collateral circulation [24]. Aortic bleeding may be spontaneous, traumatic, or iatrogenic [25].
Review of the literature regarding NF 1 aortic and iliac vasculopathy
We performed a literature review regarding the affliction of the thoracic, abdominal aorta and iliac arteries in NF1 patients using the PubMed database. We found 66 patients in total, with involvement of the thoracic aorta in 23 patients, abdominal aortic involvement in 39 patients, and isolated iliac artery involvement in 4 patients. Abdominal aortic involvement was in the form of coarctation (25 patients), aneurysmal disease (8 patients) and spontaneous rupture (6 patients). Furthermore, we found 4 published cases with retroperitoneal bleeding and fatal outcome where the diagnosis of arterial erosion from neurofibromas was set postmortem [10, 26–28]. We also found 3 other published cases where no source of bleeding could be found in laparotomy [20, 25, 29]. Detailed findings of our review in each vascular segment are the following:
Thoracic aorta
Thoracic aortic involvement included 23 patients (Table I). Thirteen of them had coarctation [5, 30–38]. In 8 cases abdominal aortic coarctation was also present, and there were multiple concomitant stenoses of visceral arteries (3 affecting the celiac axis (CA), 2 the superior mesenteric artery (SMA) and 3 affecting at least one renal artery (RA), one of which had a concomitant RA aneurysm) [5, 21, 30, 32, 35, 36]. Ten of the thirteen patients were female (aged between 10 and 20 years). Nine patients were managed with open surgical repair and all survived. One patient died before receiving treatment. Two patients underwent ET, one of which had reintervention for restenosis 15 months later [21, 38].
Table I
Reported cases of thoracic aorta involvement in patients with NF1 vasculopathy
[i] Pt – patient, M – male, F – female, CA – celiac artery, EIA – external iliac artery, SMA – superior mesenteric artery, CIA – common iliac artery, RA – renal artery, PDA – patent ductus arteriosus, SA – subclavian artery, BP – blood pressure, ePTFE – expanded polytetrafluoroethylene, AAA – abdominal aortic aneurysm, VA – vertebral artery, HR – heart rate, ICU – intensive care unit.
Four patients were found with aneurysms involving the ascending aorta, aortic arch and the proximal descending aorta [5, 39, 40]. In one ruptured aneurysm, significant intraoperative bleeding led to the patient’s death [39]. One of these patients also had an abdominal aortic aneurysm and bilateral common iliac artery aneurysms and good outcome after abdominal aortic open reconstruction [5]. The third patient was treated conservatively and was alive after 4 years and the fourth patient had a successful open repair [40]. Three patients had thoracoabdominal aneurysms. One of them was treated conservatively and the other two underwent open repair; the first later developed a new subclavian and vertebral artery aneurysm and the second died 2.6 years postoperatively of a ruptured recurrent ascending aortic aneurysm developed at the previous operating site [5]. There was 1 patient with aortic arch intramural hematoma who was treated conservatively with a successful outcome, and 2 patients with a spontaneous rupture of the aorta, one of which died before receiving treatment [41–43]. The other was a pregnant woman who was in good condition 7 years after open repair [43].
Abdominal aorta
Abdominal aortic coarctation
Isolated abdominal aortic coarctation (not involving the thoracic aorta) occurred in 25 patients (Table II) [5, 44–62]. Seven of them were treated conservatively (one of them was treated surgically for a cerebellar tumor which resolved her symptoms), 14 with open aortoplasty and/or bypass to renal and/or to mesenteric arteries (one of which was managed with supplementary stenting due to recurrence of hypertension and compression of the graft by enlarging neurofibromas). Four patients were treated with balloon renal angioplasty. One of them underwent angioplasty of the coarctated aortic segment, while 2 of them had no intervention in their mild aortic narrowing. Interestingly, one of these patients with recoarctation after initial surgical treatment exhibited dissection after stent re-dilation, which was managed with placement of numerous overlapping stents [58]. There was no mortality in all cases. In all cases blood pressure was corrected except 1 case with splenorenal bypass [44]. Re-intervention was required in 3 patients [55, 58, 62].
Table II
Reported cases of isolated abdominal aortic coarctation in patients with NF 1 vasculopathy
[i] Pt – patient, M – male, F – female, RA – renal artery, BP – blood pressure, CNS – central nervous system, IMA – inferior mesenteric artery, SMA – superior mesenteric artery, CA – celiac artery, PTFE – polytetrafluoroethylene, MAS – midaortic syndrome, L1-4 – lumbar vertebra 1 to 4, CT – computed tomography.
In 23 patients there were concomitant abnormalities in renal arteries (stenoses in 21 patients, bilateral in 14, narrowing and irregular course in 1 patient [45] and aneurysm in 1 patient [5]). Celiac axis was affected in 4 patients, SMA stenosis was present in 7 patients (one developed a post-stenotic aneurysm), detached SMA in 1 patient with retrograde flow from collateral networks [47], IMA stenosis was present in 3 patients, one after surgical correction [58] and functionally occluded in the second patient. Iliac arteries were involved in 2 patients (tortuosity in 1 patient) [45].
Spontaneous abdominal aortic rupture
Spontaneous abdominal aortic rupture was detected in 6 patients (Table III) [6, 12, 15, 23, 63, 64]. The first case of massive retroperitoneal hemorrhage due to rupture of a fragile abdominal aorta in an NF1 patient was reported by Wiger et al. in 1997 in a 35-year-old female [15]. Avulsion of the left 4th lumbar artery occurred due to a ruptured lumbar artery aneurysm. Aortic fragility prevented direct suturing during open repair and a 14 mm PTFE graft was successfully interposed. At 24 months’ follow-up no complications were detected. The second case was reported by Chew et al. in 2001 in a 34-year-old male [23]. A 3 cm long aortic tear above the aortic bifurcation along with aortic dissection was managed successfully with primary suturing. A left common iliac artery aneurysm was apparent. This is the only case where acute abdominal aortic dissection was reported. The third was reported by Hines et al. in 2002 in a 52-year-old male [63]. An aortic rupture below the renal arteries from an adjacent neurofibroma’s invasion resulted to death after failed attempts for patch angioplasty. The neurofibroma was resected but the patient died from disseminated intravascular coagulation. The fourth case was reported by Hinsch et al. in 2008 in a 28-year-old female [12]. Vascular fragility led to the patient’s death after failed attempts to repair hemorrhage from a lumbar artery as surgical manipulations resulted in further vessel injury. The fifth case was reported by Falcone et al. in 2010 in a 49-year-old female [6]. A 2.5 cm infrarenal tear from a spindle cell neurofibroma was technically successfully treated with aortic cuffs but the patient died at the 15th p.d. from anoxic brain injury. The sixth case was reported by Wang et al. in 2022 in a 41-year-old pregnant woman undergoing labor, who died due to a 5 cm tear of the abdominal aortic bifurcation which deemed irreparable intraoperatively [64]. Therefore, 7 patients were treated for spontaneous abdominal aortic rupture, 5 with OR and 2 with EVAR (including our case). Three of the 5 patients died after OR, 2 intraoperatively while 1 of the 2 patients died after EVAR.
Table III
Reported cases of spontaneous abdominal aortic rupture in patients with NF1 vasculopathy
Abdominal aortic aneurysms
Abdominal aortic aneurysms (AAA) were detected in 8 patients (Table IV) [5, 8, 14, 16, 65]. The first case of an intact AAA was reported by Oderich et al. in 2007 in a 77-year-old male [5]. OR with graft interposition was effective and a 5-year follow-up was normal. The same authors reported a second patient (74-year-old male) who died during OR repair due to a ruptured AAA. He had concomitant bilateral internal carotid and vertebral artery aneurysms. They additionally reported a third patient (68-year-old male) with concomitant thoracic and bilateral common iliac artery aneurysms, who underwent a successful aortoiliac bypass and died 4 months after the operation from unknown causes. A fourth patient (71-year-old male) reported by the same authors with aneurysmal-occlusive disease was treated successfully with aorto-bifemoral bypass, having a normal 6-year follow-up. The fifth case was reported by Park et al. in 2012 in a 49-year-old male [8]. OR was successful after EVAR performed in another institute for a ruptured aortic pseudoaneurysm. The indication for OR was a new pseudoaneurysm at the aortic bifurcation. On the 6th p.d. coil embolization was performed for a bleeding middle colic artery branch with good outcome. The sixth case was reported by Hori et al. in 2012 in a 78-year-old-male [16]. He was initially treated with EVAR for an intact aneurysm but 3 months later with OR for rupture. Perigraft lymphadenopathy and fibrotic granulomas were observed. The seventh case was reported by Morro et al. in 2019 in a 67-year-old female with a ruptured AAA (sized 3.4 cm) and concomitant aortocaval fistula who underwent EVAR and redo-EVAR on the 4th p.d. due to Ib endoleak (a coil embolization of a left IIA aneurysm was also performed) [14]. Emergency left hemicolectomy and transverse colon colostomy were performed due to rupture of 2 new left colic artery aneurysms on the 22nd p.d. with good outcome. The eighth case was reported by Nakai et al. in 2022 in a 78-year-old female [65]. She underwent a successful EVAR for a ruptured AAA (4.5 cm in diameter). A small asymptomatic pseudoaneurysm was developed at the proximal landing zone on the 7th p.d. and tracheostomy was needed due to a spontaneous cervical hematoma which later was related to a new left vertebral pseudoaneurysm. The patient survived.
Table IV
Reported cases of isolated abdominal aortic aneurysms in patients with NF1 vasculopathy
Therefore, 5 patients were treated for intact AAAs, 3 with OR and 2 with EVAR. All patients survived the first 30 days (1 died after 4 months from unknown causes). Three patients were treated for ruptured AAAs, 1 with OR who died intraoperatively and 2 with EVAR who survived. Thirty-day mortality was 0 in intact AAAs, 33% in ruptured AAAs and 57% in spontaneous aortic ruptures. Total 30-day mortality in ruptured cases (AAAs and spontaneous abdominal aortic ruptures) was 50% (5 out of 10) resembling the mortality of ruptured aneurysms in the general population. In detail, 30-day mortality was 66% in ruptured cases after OR and 25% in ruptured cases after EVAR. This superiority of EVAR in 30-day mortality may make its use more widespread in the future.
Iliac arteries
Iliac arteries were affected in combination with aortic involvement in 2 patients [5, 23]. Isolated iliac involvement has been reported in 4 patients (Table V) [5, 7, 66, 67]. The first patient with a 6-cm CIA tear died before receiving treatment [66]. The second patient with a ruptured left IIA aneurysm and an AVF was treated surgically with a femoro-femoral bypass. A newly developed aneurysm at the same site post-operatively was treated with ultrasound-guided coil embolization with good results [67]. The third patient with a right CIA aneurysm was treated conservatively with satisfactory mid-term follow-up [5]. The fourth patient with an EIA-CFA aneurysm was treated surgically. Six years later a re-do operation was performed for a profunda aneurysm with good outcome [7]. Consequently, OR repair had satisfactory results in iliac aneurysms.
Table V
Reported cases of isolated common, internal and external iliac artery aneurysms in patients with NF1 vasculopathy
Screening for NF1 vasculopathy
It is reported that vascular lesions are present in every NF1 patient if careful examination is performed and no vessel including veins is excluded [68, 69]. Some investigators suggest screening of all patients with non-invasive imaging modalities (color duplex, magnetic resonance angiography, and computed tomography scanning) [23]. Imaging must include the head, chest, and abdomen [64]. The need to assess systemically great vessels in patients with NF1 is emphasized [64]. On the other hand, other reports claim that regular vascular assessment is not recommended to all NF1 patients, as clinically significant lesions are relatively uncommon (2%). They advocate selective imaging when symptoms or clinical suspicion are apparent [5]. It is reasonable that NF1 patients should be systematically screened for vascular lesions from the third decade of life to prevent fatal complications secondary to the aneurysm rupture [70]. The mean screening interval has not been clarified but a yearly color duplex for the accessible arteries would be sensible though a whole-body CTA or MRA should be based on the physician’s judgement.
Pathology and pathophysiology of NF1 vasculopathy
The vascular fragility in NF1 is attributed to multiple mechanisms, including elastin degradation, defective smooth muscle cell function, and ischemia of the vasa vasorum, leading to medial necrosis. These changes predispose affected arteries to spontaneous dissection, aneurysm formation, and, in rare cases, complete arterial avulsion. Additionally, external compression by adjacent neurofibromas may exacerbate vessel wall instability, further increasing the risk of rupture. Arteries of any size can be afflicted in NF1. The lesions in arteries smaller than 1 mm in diameter were described by Reubi as pure intimal, intimal aneurysmal, and nodular, alone or in various combinations [28]. The proliferation of intimal spindle cells obliterates the vascular lumen. In ruptured aortas, the aortic wall is described to demonstrate medial elastolysis, mucoid degeneration, increased numbers of adventitial S 100-positive cells in one report [15] and medial thinning and degeneration of the elastic lamina, adventitial fibrosis and foreign-body granulomas in another report [8]. The observed elastolysis and medial thinning have been reported as the most likely responsible mechanisms for aneurysmal dilatation and dissection [10]. Several reports note friable vascular walls [23, 63]. Although histological evaluation is missing in several cases, the elastolysis and medial thinning described above are likely causes of arterial wall friability. Loss of neurofibromin expression in endothelial cells has been implicated in abnormal vascular smooth muscle proliferation and structural arterial fragility [10].
Extravascular pressure from neurofibromas can additionally result in luminal stenosis in larger size arteries [13], while infiltration of the wall of a large artery by a neurofibroma or ganglioneuroma has been reported to be associated with massive hemorrhage resulting in the patient’s death [10]. Cury et al. proposed two hypotheses for the causes of arterial rupture: 1) weakening of the vessel wall due to neurofibromatous invasion of the tunica media; 2) compression of the vasa vasorum of the large artery by neurofibromatous tissue, resulting in weakening of the arterial wall. Aortic disease due to adventitial compression from proliferation of Schwann cells followed by secondary changes of fibrosis presents as stenotic or occlusive disease. Alternatively, direct invasion by Schwann cells with intimal thickening and destruction of the media and elastic tissue leading to aneurysm formation may also be present [71].
Indications for treatment
As evidence is limited, no specific treatment strategies or precise indications for intervention are recommended [13]. Regarding aortic aneurysms, the actual size criteria for intervention are unknown because of the rarity of this disease. Clinical judgment is required, and treatment should be individualized [23]. Some claim that only symptomatic cases must be treated while others suggest that indications should be the same as for patients without NF1 [6]. Prophylactic percutaneous endograft relining of the infrarenal aorta to prevent aortic invasion in patients with known retroperitoneal invasion has also been suggested. The long-term effects of this approach are unknown [6]. Additionally, as plexiform neurofibromas are extremely vascular and may contain ecstatic vessels or aneurysms, preoperative embolization can minimize possible bleeding complications [10]. The European Society for Vascular Surgery 2024 Clinical Practice Guidelines recommend that the threshold diameter for considering repair in patients with AAAs and an underlying genetic cause should be individualized, depending on the underlying genetics and anatomy [26]. Of course, saccular aneurysms warrant repair regardless of their size. It is notable that the diameter of the ruptured AAAs in our review was below 5 cm in the 2 cases where the size is reported [14, 65]. This raises concerns for a decrease to the diameter threshold especially when aneurysm configuration is not thoroughly fusiform.
Treatment
The fragility of the arterial wall influences not only the potential aneurysm formation or rupture but also the type and efficacy of treatment. Open reconstruction may be successful but has been invariably associated with disastrous results as arterial clamping and suturing cause further arterial wall damage [23]. Severe perioperative complications have been reported so far, like intra- or postoperative uncontrolled bleeding. In one report of infrarenal aortic rupture, the aorta was so friable that even pledgeted sutures tore through the aortic wall and the patient eventually died [63]. In another report, a spontaneous hemorrhage of the infrarenal aorta, as a left lumbar artery torn out of the aortic wall, was successfully repaired using interrupted sutures with Teflon pledgets [15]. In open reconstruction even the self-retaining retractor may cause damage to visceral blood vessels. Thus, special attention is required regarding the retraction of the bowel and its mesentery [8]. Successful outcome was reported elsewhere, where pledgeted sutures and packing achieved safe repair in a large spontaneous tear near the aortic bifurcation [23]. Extra-anatomic bypass has been suggested with infrarenal aortic ligation, but no such report exists in the literature [6]. However, a healthy infrarenal aorta is required to achieve a safe aortic stump creation. Not only vessel friability but the extreme vascularity of the potentially surrounding neurofibromatous tissue is a concern in open surgery [23]. Large neurofibromas have a gelatinous consistency and thus fragment easily after surgical manipulations. The friable vessels tear and avulse easily from each other with profuse bleeding and ligatures and electrocautery may not achieve effective hemostasis [63, 72]. In some cases, aneurysmal ligation and bypass grafting is preferable, in contrast to direct repair, to avoid the infiltrating vascular neurofibromatous tissues [23]. If open surgery is going to be used, specific repair techniques to avoid iatrogenic vessel injury are needed, like delicate and atraumatic handling of tissues, careful positioning of retractors and use of soft and protected arterial clamps. Moreover, grossly healthy-appearing aortic segments at anastomotic sites must be used. Sewing the anastomoses with pledgeted sutures, and use of supporting cuffs and glues are also needed [5, 8, 65, 73]. Overall, open surgical repair in NF1 patients presents unique challenges due to the friability of vessel walls, increased risk of anastomotic dehiscence, and potential interference from adjacent neurofibromas. While OR remains an option for anatomically unfavorable cases, endovascular repair (EVAR) offers a minimally invasive alternative with reduced perioperative morbidity in these high-risk patients.
On the other hand, endovascular repair has uncertain durability in the future due to the diffuse and progressive nature of NF1 vasculopathy [74]. It may cause intimal tears or secondary pseudoaneurysm formation due to radial and spring back forces of the stent graft against a fragile wall, which usually require additional treatment [6, 8, 14, 65, 74]. Careful manipulation of wires is also recommended as these vessels may be vulnerable to dissection [6]. The first case of ET of arterial rupture in an NF1 patient was described by Falcone et al. [6]. A spontaneous infrarenal aortic rupture was treated with EVAR and an intimal erosion at the inferior level of the endograft was found postmortem. A neurofibroma which had infiltrated the wall of the aorta was the culprit lesion [6]. In another case, 3 months after EVAR, periaortic lymphadenopathy caused deformation of the aneurysm, and the endograft migrated and penetrated the wall. Open repair was successful [16]. The long-term reaction of the friable aortic wall to stent-grafting and the durability of prevention on vascular wall invasion remains unknown [6]. Currently there is no consensus as to which type of treatment is better. Traditionally, the presence of a genetic or heritable aortic condition has been considered a contraindication to endovascular intervention [17]. ESVES guidelines recommend as the first option, open surgical repair for abdominal aortic aneurysms in young patients with suspected connective tissue disorders [73]. However, EVAR may be offered in the emergency setting as it is associated with decreased morbidity and mortality compared to open surgery, even if it is a bridging procedure to a more definitive repair [17]. It would also be worth considering for patients who are not candidates for open surgery, who are at high risk for reintervention, or who have a previous graft implantation or multiple redo procedures even if they have a genetic or heritable aortic condition [17]. For these reasons a gradual move towards endovascular repair has been observed [73]. However, EVAR cannot yet be recommended for routine use in patients with underlying genetic causes and predisposition to aortic fragility and continued aortic dilatation as its durability is uncertain [73]. Nevertheless, management in patients with an underlying genetic cause should be carried out in a highly specialized center by a multidisciplinary aortic team [17]. Nowadays, it remains controversial whether endovascular or open surgery is appropriate for NF1 patients with aortic pathology AAA [8, 14, 23, 65]. While EVAR was deemed the most suitable approach in this case, open repair (OR) remains an alternative, particularly in younger patients with favorable anatomy. However, NF1-related vascular pathology presents unique challenges for OR, including increased tissue friability, a higher risk of perioperative complications, and potential difficulty in achieving durable anastomoses. In addition to EVAR, adjunctive endovascular techniques, such as coil embolization of the avulsed IMA or the use of covered stents, could also be considered depending on the extent of vessel injury and aneurysm characteristics.
As we mentioned above, postoperative complications due to arterial fragility have been reported after EVAR, like aortic wall injury, development of new (secondary) ruptured aneurysms in a splanchnic artery or unpredictable bleeding at remote sites [6, 8, 65]. Sometimes bleeding occurs in areas where previous operations have been performed. In one report, bleeding from a disrupted paraspinal artery occurred postoperatively in a remote site of a previous orthopedic procedure for scoliosis [10]. Intraluminal tumor and thrombus were found in the artery postmortem [10].
Regarding spontaneous bleeding and aneurysms of other arteries, ET with coil embolization or percutaneous stent graft placement, are often considered preferable when it is mandatory to maintain an efficient blood flow in the regions perfused by the targeted vessel. This approach is less invasive and has low intra-operative and post-operative mortality [74]. Although, there are concerns about the increased risk of complications with diagnostic angiography and other catheter-based procedures in NF1 patients, in a recent systematic review, it is concluded that ET is safe and effective even in hemodynamically unstable NF patients at all ages [74]. Notably, this review did not include aortic pathology [74]. Finally, it is worth mentioning that no case was encountered in thoracic aorta with primary aortic dissection. In one reported case, a Stanford type B aortic dissection was a complication of percutaneous intercostal aneurysm embolization with good outcome under medical treatment [75].
To sum up, previous reports have highlighted the variability in outcomes between EVAR and OR in NF1-related vascular emergencies. While OR offers definitive repair, it is associated with higher morbidity due to increased surgical complexity in these fragile vessels. EVAR, on the other hand, has demonstrated promising results in achieving immediate hemostasis with a lower perioperative risk, although concerns regarding long-term durability persist. A comparative analysis of available cases suggests that patient selection is critical, with EVAR favored in high-risk surgical candidates and anatomically feasible cases.
Survival
Patients with NF1 die at a median age of 59 years. That means that they die 15 years younger than controls matched for age and sex [76]. Overall patient survival is 77% at 10 years in contrast to 87% for the expected survival of a matched population [5]. The most common cause of death is malignancy. Vascular disorders are the second cause of death, especially among those patients aged 40 years old [5, 76, 77].
Follow-up
Lifelong surveillance is important after EVAR or TEVAR as potential continued expansion of the aneurysm and the vulnerable aorta at the native proximal and distal landing zones may occur [17, 77]. Consequently, any new intimal tears, endoleaks, dissections or endograft migration necessitate repeat interventions in up to 35% of cases [17]. Given the progressive nature of NF1-related vasculopathy, long-term follow-up with periodic CTA/MRA is crucial. Additionally, optimizing blood pressure control and considering adjunctive medical therapy may help reduce arterial wall stress and minimize future vascular complications. In our case, although early postoperative imaging confirmed technical success, long-term surveillance remains crucial due to the risk of delayed complications, including graft migration, endoleak formation, and the development of new aneurysms. The patient was scheduled for routine follow-up with CTA at 6 months and annually thereafter to monitor the stability of the repair and assess for potential disease progression. In our opinion, postoperative surveillance should be identical with that suggested from the ESVES guidelines after EVAR, mainly including a yearly imaging evaluation [26].
Conclusions
NF1 patients present distinct challenges regarding treatment of aortic pathology. Although endovascular treatment is not the first choice in these patients presenting with aortic aneurysm or spontaneous ruptures, it may be valuable in urgent cases, even as a bridging procedure, or in redo operations or in high-risk patients. On the other hand, open surgery carries its own risks due to vascular friability, therefore special care and particular surgical measures are needed.




