Introduction
Acute myocardial infarction (AMI) is a major killer among adults. While only a small fraction of cases involves younger patients, several studies have hinted that the number could be rising. Different pathways and mechanisms including coronary artery spasms, abnormal anatomy of the coronary arteries, systemic inflammatory disease, or factors contributing to endothelial damage such as hypertension, can all trigger AMI in younger age groups [1].
There is a lack of recent data on the cases of AMI and various patient characteristics and outcomes among teenagers. Since typical symptoms of AMI are often ignored in such age groups, it is vital that potential risk factors are identified. This also avoids the need for costly diagnostic testing in patients with low probability [2]. We hereby conducted a retrospective analysis using the biggest inpatient database in the United States.
Material and methods
Data source
In this study, the National Inpatient Sample (NIS) data sets for the years 2016–2020 were utilized. The NIS is considered to be one of the most extensive hospitalization records in the United States via the Healthcare Cost and Utilization Project (HCUP), the Agency for Healthcare Research and Quality (AHRQ), and partners. It encompasses at least 95% of the hospitalization in the country, and currently there are 48 states and the District of Columbia participating in it. The database has undergone many revisions over the years, making it a very accurate means of conducting different types of analysis. It also provides a self-weighting design that allows the user to adjust the data for national estimates. The database consists of different patient and hospital characteristics. The use of International Classification of Diseases (ICD) codes allows users to identify procedures and different conditions [3].
Study population
We first included patients classified as teenagers in our study (ages 13–19 years inclusive). A diagnosis of acute myocardial infarction was identified via their International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes I21.x-22.x, as recommended in past studies [4, 5].
Analysis and outcomes
The number of AMI cases were compared per year, and linear-to-linear analysis was applied to evaluate changes in trend over the 5-year period. Various patient characteristics were compared via χ2 tests. Logistic regression models were also used to estimate the adjusted odds ratio of recording a diagnosis of AMI among teenagers based on the presence of different characteristics and comorbidities. Finally, multiple outcomes such as the use of extracorporeal membrane oxygenation (ECMO), coronary artery bypass graft surgery (CABG), percutaneous coronary intervention (PCI), and events of cardiogenic shock or mortality were also studied, and the adjusted odds ratio of mortality among teenagers was calculated relative to non-AMI admissions.
Statistical analysis
All statistical analyses for our study were performed via SPSS 29.0 (IBM Corp., Armonk, New York). A p-value less than 0.05 was considered significant. Results of logistic regression analyses were reported as an adjusted odd ratio (aOR) along with the 95% confidence interval (CI).
Ethical clearance
The NIS was released in a de-identified form, with no personal information that would allow the patients to be tracked. The HCUP also forbids the reporting of any data cell less than 11, and its DUA waives the need for ethical clearance or IRB approval.
Data availability
The National Inpatient Sample (NIS), used in our study for the analysis, can be obtained by contacting the Healthcare Cost and Utilization Project (HCUP) (https://www.hcup-us.ahrq.gov/nisoverview.jsp).
Results
Baseline characteristics
In the United States, between 2016 and 2020, there were a total of 4,064,189 admissions among teenagers, which included 2170 hospitalizations that also recorded a diagnosis of acute myocardial infarction (53.3 cases per 100,000 admissions among teenagers) (Table I). Among these, 82.0% had a diagnosis of NSTEMI. The mean age was 18.13 years (vs. 16.77 years for other causes), with a mean length of stay of 8.21 days (vs. 4.44 days for other causes, p < 0.01). In addition, the number of cases of AMI per 100,000 hospitalization records increased between 2016 to 2020, nearly doubling, from 40.6 per 100,000 in 2016 to 80.7 per 100,000 in 2020 (ptrend < 0.01).
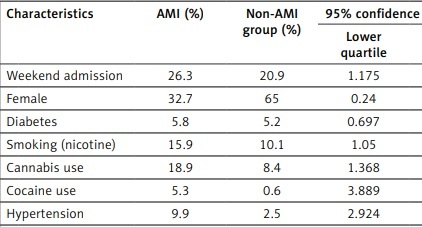
Table I
Characteristics of teenagers admitted with a diagnosis of acute myocardial infarction in the United States
Admissions for teenagers with AMI is more likely to be on weekends (26.3% vs. 20.9%, aOR = 1.298, 95% CI: 1.175–1.434, p < 0.001), among those who have a history of smoking (15.9% vs. 10.1%, aOR = 1.198, 95% CI: 1.05–1.367, p = 0.007), cannabis use (18.9% vs. 8.4%, aOR = 1.558, 95% CI: 1.368–1.774, p < 0.001), or cocaine use (5.3% vs. 0.6%, aOR = 4.841, 95% CI: 3.889–6.027, p < 0.001). While a higher proportion of teenagers who needed admission for non-AMI causes were females (32.7%), females were less likely to have a diagnosis of AMI (32.7% vs. 65%, aOR = 0.264, 95% CI: 0.24–0.291, p < 0.001). Furthermore, admissions were more likely to include teenagers with hypertension (9.9% vs. 2.5%, aOR = 3.382, 95% CI: 2.924–3.913, p < 0.001). Teenagers who were not covered by Medicaid or private insurances were also more likely to be admitted for AMI compared to Medicaid beneficiaries (12.4% vs. 8.2%, aOR = 1.278, 95% CI: 1.108–1.476, p < 0.001). Several racial differences were also seen as AMI in teenagers was more likely to involve Blacks (24.3% vs. 19.4%, aOR = 1.37, 95% CI: 1.221–1.538, p < 0.001) compared to Whites. Finally, our analysis did not find any socioeconomic differences as median household income quartiles did not influence the odds of a teenager being admitted for AMI. Similarly, diabetes among teenagers, and private insurance beneficiaries, Hispanics, those of races other than White, Black, or Hispanic did not have any statistical association with the odds of AMI in teenagers.
Outcomes
A total of 180 (8.3%) patients also recorded an event of cardiogenic shock during their hospitalization. Fifteen (0.7%) cases required CABG, 90 (4.1%) cases underwent PCI, while 60 (2.8%) required ECMO. Unfortunately, 270 (12.5%) teenagers who were hospitalized with a diagnosis of AMI did not survive.
Discussion
Our study provides the largest and most recent analysis for the incidence, characteristics, and outcomes of teenagers with acute myocardial infarction. The rate of AMI cases per 100,000 hospitalization records in general has been rising. This further highlights various potential problems among teenagers, which can be linked with the rise in various substance abuse [6]. As a matter of fact, our study found that teenagers with AMI were more likely to be those who smoke, or use cannabis or cocaine. Cannabis is known to alter blood flow to the heart and activate the sympathetic system. This provokes a higher demand of blood, which cannot be fully met [7]. Meanwhile, cocaine can trigger coronary artery vasospasm that reduces blood flow to the heart. It can also upregulate the sympathetic system, leading to a rise in heart rate and contractility, and thus to a rise in oxygen demand [7, 8]. Smoking plays an important role in atherogenesis, and various studies have reported events of AMI in young adults even with normal coronary arteries [9]. Our study thus confirms the findings previously reported by several small sample studies on the event and the impact of these substances among teenagers and young adults. However, further studies can help evaluate the causative and associative roles of these risk factors in these patients [10, 11].
Furthermore, a male predominance was noted, and an increased risk was seen among males compared to females. Male adolescents and teenagers are more likely to be exposed to various risk factors. In a recent study, 16.5% of male adolescents reported to be smokers, compared to only 1.9% of females [12]. Similar findings have also been reported among cannabis users; 26.6% of males (vs. 9.8% of females) between the ages of 13 and 17 years were frequent users [13]. In addition, our study highlighted the impact of weekend admission, which is often believed to include more severe patients [14, 15]. Finally, another risk factor was the presence of hypertension. The role of hypertension has been highly elaborated in the literature because it can trigger damage and various vascular insults that form part of the pathophysiology of AMI. A recent analysis from Hardy et al. also noted that the blood pressure levels among children and adolescents in the United States increased between 2015 and 2018 [16].
Several racial and socioeconomic differences were also reported in our analysis. While a higher percentage of AMI cases were classified as White, the odds of the event was higher among Black teenagers. The higher percentage reflects the higher census-based distribution of American teenagers, with a higher percentage being racially White. Our findings on racial disparities differ from a past study on adolescents that used the 1998–2001 NIS that failed to find any racial disparities at that time [2]. The higher odds of AMI among Black teenagers should also be further investigated. While the disparities may be linked with any racial predisposition (if any) or risk factor linked with the pathophysiology of AMI, social causes such as awareness and access to various external risk factors should also be studied. This can help us understand the differences seen between the 2 studies that are now 2 decades apart, and a better understanding can help alleviate such impact and lower the incidence of AMI among them [17, 18]. Further studies may help better understand the causes, and effective ways to tackle these differences can be implemented.
Our analysis failed to find differences in the odds of AMI among teenagers based on median household incomes and on various factors such as diabetes. The impact of diabetes is insidious and thus was not statistically significant in younger patients. Due to the lack of adequate data from different countries and facilities, we are unable to compare the incidence rate of AMI among teenagers, the mortality rates, and the rates of teenagers with AMI requiring CABG or PCI. Moreover, because the database does not allow users to ascertain several factors such as medications being used, levels of troponin, and other laboratory findings, future studies in a clinical setting are encouraged to further investigate the results of our study. Moreover, the database uses a coding system, which can be prone to errors due to misclassification or coding by phisicians. Over the years, HCUP has adopted several measures to limit the impact of such shortcomings and make the database more accurate.
In conclusion, our study found that a teenager is more likely to be hospitalized for AMI if that person is admitted on a weekend, is a smoker, uses cannabis or cocaine, has hypertension, is covered by forms of insurance other than Medicaid or private, or is racially Black, while lower odds were seen in females compared to males.