Introduction
Stroke, a prominent global cause of mortality and disability, is broadly categorized into ischemic and hemorrhagic types. Ischemic stroke, which accounts for approximately 71% of cases worldwide, has evolved from a primarily clinical definition to a tissue-based classification, facilitated by advances in brain imaging [1]. Transient ischemic attack (TIA), a temporary interruption of blood flow without permanent injury, shares pathogenesis and research approaches with ischemic stroke [2]. Experiments in the 1970s revealed that the initial clinical deficit in stroke patients arises from a perfused, hibernating brain region called the ischemic hemisphere [3]. The discovery that early reperfusion can save this area laid the groundwork for transformative reperfusion therapies after the positive stroke thrombolysis trial in 1995 [4]. Optimal management of ischemic stroke involves multidisciplinary teams in dedicated stroke units adhering to evidence-based guidelines. Intravenous thrombolysis, effective within 4.5 h of stroke onset, may be extended to 9 h or for awakening strokes with favorable cerebral perfusion imaging. Endovascular thrombectomy, beneficial within 6 h or up to 24 h with cerebral perfusion imaging, treats large-vessel occlusion. Timeliness is crucial, emphasizing the imperative to optimize the health system to maximize therapeutic benefits [5–13].
Stroke, encompassing both ischemic and hemorrhagic types, affects a staggering 13.7 million individuals globally annually, ranking as the second leading cause of death with 5.5 million fatalities [14, 15]. Approximately 1 in 4 adults will experience a stroke in their lifetime, contributing to over 80 million stroke survivors worldwide [2, 15]. This survivor cohort constitutes a high-risk population and is a primary focus for secondary prevention strategies.
An epidemiological survey of stroke and its risk factors can help identify individuals at higher risk and therefore promote stroke prevention strategies. The aim of this study was to estimate the current prevalence of stroke and evaluate stroke associated risk factors in Albania.
Material and methods
Ethics board approval was waived for this analysis. This was a single-center retrospective analysis conducted in Albania for the period from May 2015 to September 2021. Data were collected retrospectively through hospital records. Stroke was defined as sudden onset of a nonconvulsive and focal neurological deficit, and ischemic stroke was diagnosed using brain computed tomography (CT), magnetic resonance (MR) imaging, or both.
We examined patient history characteristics encompassing demographics, stroke history, conventional vascular risk factors, and lifestyle-related risk factors. A history of stroke was defined as a precedent occurrence of ischemic or hemorrhagic stroke preceding hospitalization for the ischemic stroke index. Conventional vascular risk factors included hypertension, diabetes mellitus, and dyslipidemia. Lifestyle-related risk factors included smoking, alcohol consumption, and obesity. Definitions for risk factors were as follows: hypertension (systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg chronically or pre-stroke treatment with antihypertensive drugs), diabetes mellitus (fasting blood glucose concentration ≥ 7.0 mmol/l, occasional blood glucose concentration ≥ 11.1 mmol/l, positive 75 g oral glucose tolerance test, or glycated hemoglobin A1c concentration ≥ 6.5% on two different days during hospitalization or at the chronic stage, or pre-stroke treatment with antidiabetic drugs), dyslipidemia (either low-density lipoprotein-cholesterol level ≥ 3.62 mmol/l, high-density lipoprotein-cholesterol level ≤ 1.03 mmol/l, triglyceride level ≥ 1.69 mmol/l, or pre-stroke treatment with a cholesterol-lowering drug), smoking (prior or current cigarette smoking), drinking (habitual consumption of alcoholic beverages), and obesity (body mass index ≥ 25 kg/m2). Body mass index was calculated based on measurements taken at admission of body weight and height. Carotid stenosis was delineated as a constriction exceeding 50% and was diagnosed through ultrasound imaging. Patients underwent a one-month follow-up following the initial stroke through comprehensive physical examinations.
Results
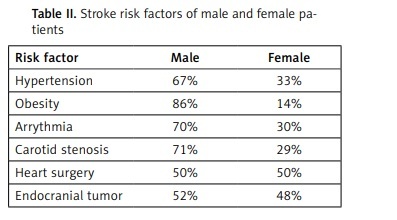
The mean age of the 3860 patients was 74.6 ±10.4 years, and 73.5% were men. The prevalence of risk factors is documented in Table I, outlining the frequency of each within the studied cohort (Table I). The prevalence rates of carotid stenosis, arrythmia, obesity and hypertension were significantly higher in males than in females (p < 0.001) (Table II). Out of the 3860 patients in the study cohort, 641 (16.6%) subjects died, while 335 (8.7%) patients achieved complete recovery. Hemiparesis was observed in 386 (10%) patients and hemiplegia in 868 (22.4%) patients.
Discussion
In 2016, the global incidence of ischemic stroke was reported at 9.5 million cases. Correspondingly, in 2017, there were 2.7 million deaths attributed to ischemic stroke [2, 16, 17]. Over the period from 1990 to 2013, there was a decrease in global incidence, mortality, and disability-adjusted life years for ischemic stroke, although the prevalence exhibited fluctuations, increasing from 1990 to 2005 and subsequently decreasing until 2013 [17]. The nuanced changes in prevalence are attributed to reductions in stroke mortality, improved secondary prevention, and enhanced stroke detection [18].
Non-modifiable risk factors for ischemic stroke include age, sex, and genetic predispositions. Age-related influences on stroke risk differ between developed and developing countries [17], with steeper increases observed in developed nations after the age of 49. The prevalence of ischemic stroke nearly doubled globally among those aged 20 to 64 from 1990 to 2013 [17–20]. The incidence is higher in men compared to women. While some monogenic causes of ischemic stroke have been identified, such as CADASIL and CARASIL, the majority of cases are sporadic, with an estimated heritability of 37.9% [21].
Modifiable risk factors, as identified in the INTERSTROKE study, contribute significantly to the population-attributable risk for ischemic stroke. These factors include hypertension, low physical activity, unfavorable apolipoprotein B-to-ApoA1 ratio, dietary habits, central obesity, psychosocial stress, smoking, cardiac causes (atrial fibrillation, previous myocardial infarction), high alcohol consumption, and diabetes mellitus [22]. Notably, self-reported hypertension or a blood pressure exceeding 160/90 mm Hg carries the strongest risk [22]. Other potential risk factors include sleep apnea, chronic inflammation, periodontal disease, chronic kidney disease, and associations with transient increases in stroke incidence due to air pollution exposure [23–27].
Between 1990 and 2010, ischemic stroke trends diverged by income level. High-income countries experienced declines in incidence, mortality, disability-adjusted life years, and mortality-to-incidence ratio. Conversely, low-income and middle-income nations showed no significant changes. The disparities may stem from variations in population demographics, life expectancy, health status, and healthcare standards [18].
Albania’s inaugural national health report in 2014 reveals compelling evidence of a notable increase in cerebrovascular disease mortality over the preceding two decades. Strikingly, Albania is the sole Southeastern European country exhibiting such an escalation. This distinctive trend raises concerns among health professionals and policymakers, highlighting unique challenges in this transitional nation [28]. According to the literature, all Central and East European countries experienced a decline in all-cause disease burden between 1990 and 2019, and a gap was confirmed between the East, the Central, and the West European region for men but not for women [29]. The WHO estimated that non-communicable diseases (NCDs) account for about of 90% of the deaths in Albania and the probability of dying between ages 30 and 70 years from the 4 main NCDs is about 19%. Cardiovascular disease is the top cause of mortality in Albania, accounting for 59% of all deaths. According to the GBD 2010 Study, the three main risk factors responsible for the majority of the burden of disease in 2010 in Albania were dietary risk factors, hypertension and smoking. Overall lifestyle factors accounted for more than 70% of the total burden of disease in Albania, whereas dietary risk factors alone were accounted for 38% of the total mortality in Albania [30].
Examination of stroke patient records in our analysis revealed a male predominance, reflected in a ratio of 2.2 : 1. Notably, carotid and vertebral artery stenosis emerges as a substantial etiological factor, emphasizing the potential life-saving impact of early diagnosis and surgical intervention. Hypertension stands out as the prevailing chronic comorbidity, underscoring the imperative for comprehensive medical interventions, particularly given the persistently elevated mortality rates. Strategic interventions, such as stringent hypertension control, management of cardiac rhythm disorders, adherence to a health-conscious lifestyle, and abstinence from smoking and excessive alcohol consumption or effective management of dyslipidemia, constitute focal points in medical recommendations. Urgency in addressing diagnosed carotid artery stenoses through prompt surgical or endovascular interventions is underscored, offering crucial avenues to mitigate fatalities and ensure the well-being of individuals at risk of stroke. Nevertheless, it is imperative to acknowledge that social and economic factors in Albania pose substantial barriers to the timely diagnosis and intervention in these cases, necessitating comprehensive strategies to address these systemic challenges. This comprehensive analysis underscores the need for prospective trials in Albania to further investigate the efficacy and optimal timing of strategic interventions, such as hypertension control and surgical procedures, while acknowledging and addressing the significant impact of social and economic factors on timely diagnosis and intervention.
A key limitation of this study is its exclusive reliance on a single-center retrospective analysis. This constraint limits the generalizability of findings to a broader population, as outcomes may be influenced by institution-specific factors. The retrospective design introduces inherent biases and hinders the establishment of causal relationships. Despite these limitations, the study provides valuable insights within its defined scope, and findings should be interpreted considering these constraints.
In conclusion, our analysis underscores the male predominance (2.2 : 1) in stroke cases. Carotid and vertebral artery stenosis is a significant factor, emphasizing the life-saving potential of early intervention. Hypertension prevalence highlights the need for comprehensive medical strategies, including lifestyle changes. Urgent management of diagnosed carotid artery stenoses is vital. Social and economic factors in Albania pose challenges, demanding comprehensive strategies. Prospective trials are crucial to explore intervention efficacy and timing, and address socioeconomic impacts on timely stroke management.