Introduction
Peripheral arterial disease (PAD) refers to atherosclerosis involving the aorta, iliac artery, and lower limb arteries. PAD affects 10–15% of the global population, including approximately 20% of those aged > 60 years [1]. The global incidence of PAD has increased from 164 million in 2000 to 202 million in 2010 [2]. Diabetes mellitus and smoking are the main risk factors for symptomatic PAD, while other risk factors include advanced age and male sex [3]. In recent years, PAD has become an indicator of generalized atherosclerosis [4–6].
In the early stage, PAD is often asymptomatic. Its clinical manifestations range from intermittent claudication to critical ischemia. Patients with PAD-LL have decreased arterial perfusion, commonly referred to as “poor circulation in the lower limbs.” In most cases, atherosclerotic plaques limit artery flow, which restricts blood supply to the more distal extremities (Figure 1).
Figure 1
Pathophysiology of peripheral arterial disease of lower limbs. Credits to: Rodrigo Tonan (medical illustrator)

The evaluation of patients with PAD-LL consists of a physical examination, in which ankle-brachial index (ABI) measurements are obtained, as well as clinical and non-invasive instrumental tests, including color Doppler ultrasonography or more sophisticated methods, such as transcutaneous oxygen pressure (TCPO2) [7] and near-infrared spectroscopy (NIRS) [8–10]. Infrared thermography (IRT) is a non-contact, non-invasive, low-cost, and easy-to-use tool that measures the temperature dissipated by the skin, which directly depends on the quality of tissue blood perfusion. Obstruction of the arterial vessels reduces tissue blood perfusion, compromises cell metabolism, and thereby decreases heat production.
Human thermoregulation occurs in response to changes in core and skin temperature. Cutaneous circulation is one of the main effectors of human thermoregulation. During thermal stress, increases in core and skin temperatures lead to cutaneous vasodilation through combinations of neural mechanisms and the local effects of higher temperatures on skin vessels [11]. During cold stress, reduced temperatures lead to cutaneous vasoconstriction through combined neural and local mechanisms. Under normothermic conditions, skin blood flow comprises approximately 5% of the cardiac output, on average. However, the absolute amount of blood in the skin can range from almost zero during periods of maximum vasoconstriction (such as during cold stress) to 60% of the cardiac output distributed over the body surface during maximum vasodilation (in heat stress) [12]. Skin pigmentation does not affect thermal emission [13].
IRT has been used to study diseases in which skin temperature could reflect the presence of inflamed underlying tissues or could indicate increases or decreases in blood flow due to a clinical abnormality [14], which are mostly related to changes in density, composition, volume, and temperature. IRT can reveal small physiological changes in body temperature homeostasis. This technique defines and assesses the physiological state of the tissue examined through thermal mapping based on the emission of infrared radiation, which can provide valuable information for medical diagnosis. There is growing interest in IRT within the medical field, as this technique has good potential for use in various applications, including diagnostic, prognostic, biometric, patient monitoring, and surgical purposes [11]. For example, studies have demonstrated the usefulness of IRT in situations of acute lower limb ischemia [15–17], diabetic foot complications [18, 19], and in monitoring patients undergoing percutaneous transluminal angioplasty [20, 21]. Recently, an IRT camera connected to a smartphone (transforming it into a thermographic camera) was used to effectively diagnose acute lower limb ischemia [15–17].
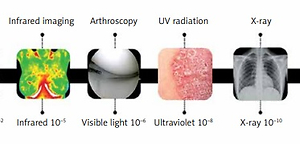
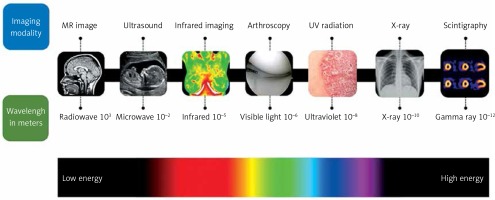
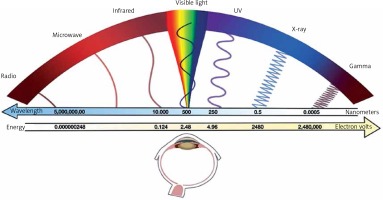
IRT is based on the concept that all objects with temperatures above absolute zero emit electromagnetic radiation [22]; thus, an increase in temperature leads to an increase in radiation levels [23]. Typically, this radiation is within the infrared band, invisible to humans, and has wavelengths between 0.8 µm and 14 µm [24–26] (Figure 2). IRT detects the infrared radiation emitted by the body’s surface and quantifies changes in body temperature, ultimately leading to changes in blood flow. Most diagnostic imaging instruments use specific portions of the electromagnetic spectrum (Figure 3) [11]. However, unlike other medical instruments, IRT is not radioactive, making it safe for use and presenting a wide range of possible applications in medicine, especially in diagnosing diseases that affect an individual’s thermal homeostasis.
Figure 2
Electromagnetic spectrum (visible and infrared portions). Credits to: Alamy Stock Photo (Image copyrighted for reproduction in magazines and books)
This study aimed to assess whether IRT with a portable camera can be a valuable tool for the diagnosis or screening of PAD-LL when compared to the traditional method of color Doppler ultrasonography.
Material and methods
We conducted an analytical observational study with a cross-sectional design. Exclusion criteria were patients with (1) a history of surgical revascularization or percutaneous transluminal angioplasty of a lower limb as they were expected to have normal or slightly altered thermograms; (2) a diagnosis of atrial fibrillation, which impairs assessments with color Doppler ultrasonography, IRT, and ABI measurement; (3) significant varicose disease of the lower limb, which, owing to blood stasis, could interfere with thermal mapping of the lower limbs; (4) total or partial amputation of the lower limb, which could render comparative evaluation impossible; or (5) current ulceration or infection in the lower limb, which could increase the local temperature and impair the thermogram evaluation.
From December 2019 to November 2020, we evaluated 105 volunteers (55 aged over 18 years) selected from the Vascular Surgery Outpatient Clinic of the University Hospital of Brasília.
Three participants with atrial fibrillation, four with ulceration/infection, one with amputation of the fingers, and two who had undergone percutaneous treatment (angioplasty) were excluded, leaving 45 eligible for the study (PAD-LL group). Forty-five volunteers over 18 years of age were also screened; these volunteers did not present with PAD-LL and met the criteria for inclusion (control group).
All participants signed an informed consent form prior to enrollment in the study, which was written in accordance with the principles of the Declaration of Helsinki and its later amendments. The Research Ethics Committee of the University of Brasília approved the study (CAAE, registered at the Brazilian Ministry of Health under project number 20621618.8.0000.5558).
Data on demographics, personal and family medical history, current medications, and cardiovascular risk factors (body mass index (BMI), smoking, diabetes, and hypertension) were recorded for each participant. Continuous-wave Doppler (8 MHz; DF 7001 VN, Medpej; Ribeirão Preto, São Paulo, Brazil) was used to measure the systolic blood pressure in the four extremities following current guidelines, and the ABI was calculated based on these measurements [27, 28].
The PAD-LL group consisted of volunteers with an outpatient diagnosis of peripheral arterial disease by color Doppler ultrasonography. However, for standardization purposes, both groups underwent arterial Doppler imaging of the lower limbs to confirm the disease in the PAD-LL group and the normal state of circulation of the lower limbs in the control group. Color Doppler ultrasonography of the lower limbs was performed with a portable device (M-Turbo, Sonosite/Fujifilm; Bothell, Washington, USA) with a linear transducer (HFL38X/13–16 MHz). Two physicians with experience in Doppler ultrasound independently evaluated the patients’ lower extremities to minimize the examiner effect. Discrepant results were then arbitrated by a consensus.
PAD was considered as the presence of a clinically relevant lesion on color Doppler ultrasonography (stenoses above 50% and total occlusions).
Then, infrared thermal images of the lower limbs were obtained. All images were acquired using a Flir C3 portable digital camera (FLIR Systems AB, Danderyd, Sweden), weighing 130 g and equipped with an 80 × 60 infrared sensor (4 800 pixels) with good thermal sensitivity (i.e., resolution below 0.10°C). Thermograms were analyzed using the Thermidas Imager (Thermidas Ltd, Tampere, Finland) and FLIR ResearchIR (FLIR Systems Inc.) programs.
A thermogram showing a temperature difference greater than 2.00°C between two points on any lower limb (including the feet) or between both was defined as altered. For these analyses, each segment was divided into the areas above (suprapopliteal) and below (infrapopliteal) the knee. Thermal images were obtained at ambient temperatures ranging from 22°C to 24°C. Each participant was initially placed in the supine position for 15 to 20 min to reach thermal equilibrium. Each test was performed with the participant in the standing position, with thermal images obtained from the front and back. The infrared camera was placed on a tripod one meter from each participant’s feet.
Statistical analysis
Continuous variables, including age, BMI, and ABI, were found to be normally distributed using the Kolmogorov-Smirnov test and are expressed as the mean ± standard deviation. Comparisons between groups were performed using the t-test for continuous variables and Pearson’s chi-square test (χ2) for categorical variables. Statistical significance was set at a threshold of p ≤ 0.05. All data were analyzed using IBM SPSS Statistics software (version 20.0; IBM Corp., USA).
Results
The current study enrolled 45 participants diagnosed with PAD-LL, with an average age of 58.29 ±9.08 years (26 women and 19 men), while the control group consisted of 45 participants without PAD-LL, with an average age of 59.78 ±7.35 years (25 women and 20 men). The age distribution (p = 0.394; t-test) and the ratio between men and women (p = 0.831; χ2 test) showed no statistically significant differences between the control and PAD-LL groups. Table I presents the medical and demographic characteristics of each group.
Table I
Baseline characteristics of the enrolled study participants
| Characteristics | Control (n = 45) | PAD-LL (n = 45) | P-value |
|---|---|---|---|
| Age, mean (SD) [years] | 59.78 (7.35) | 58.29 (9.08) | 0.395* |
| Male (n)/Female (n) | 19/26 | 20/25 | 0.831** |
| Body mass index, mean (SD) [kg/m2] | 24.83 | 26.5 | 0.001* |
| Ankle-brachial index, mean (SD) | 0.94 | 0.88 | < 0.001* |
| Current or previous smoking, no (n)/yes (n) | 30/15 | 16/29 | 0.003** |
| Hypertension, no (n)/yes (n) | 23/22 | 24/21 | 0.833** |
| Diabetes mellitus, no (n)/yes (n) | 25/20 | 13/32 | < 0.001** |
An analysis of the demographic and medical characteristics within each group showed that BMI, ABI, current or previous smoking, and a diagnosis of diabetes mellitus were significantly more prevalent in the PAD-LL group than in the control group (Table I).
The use of IRT as a diagnostic tool in medicine, especially in PAD, is still recent. The definition of an altered thermogram varies between studies. For this purpose, a pilot study was previously carried out with gradients of 1.0, 1.5, 2.0, 2.5 and 3.0°C. The 2.0°C gradient was the one that presented the best correlation with PAD-LL.
In the PAD-LL group, 38 participants presented with altered thermograms, while the remaining seven presented with normal thermograms. In the control group, 44 participants presented with normal thermograms, and one presented with an altered thermogram. Based on these results, IRT showed a sensitivity of 97.62%, a specificity of 91.67%, a positive predictive value of 91.11%, and a negative predictive value of 97.78% for the diagnosis of PAD-LL when compared to color Doppler ultrasound.
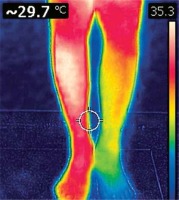
Figure 4 illustrates the thermogram of a patient with occlusion of the left popliteal artery. The change in pattern from red to yellow and more distally to blue corresponds to compromised tissue perfusion.
Among the 38 altered thermograms in the PAD-LL group, 35 were in the region below the knee. The only altered thermogram in the control group was in the region above the knee (p < 0.0001; χ2 test).
In both groups, ABI was divided into two categories, ≤ 0.90 (altered) and > 0.90 (normal). In the PAD-LL group, 31 participants showed an ABI ≤ 0.90, and 14 had an ABI > 0.90. In the control group, 42 patients presented with an ABI > 0.90, and three presented with an ABI ≤ 0.90. Based on these results, ABI showed a sensitivity of 91.17%, a specificity of 75,00%, a positive predictive value of 68.89%, and a negative predictive value of 93.33% for PAD-LL diagnosis when compared to color Doppler ultrasound.
Discussion
As the arteries progress distally in the lower limb, they divide and decrease in size to provide arterial supply to the entire limb. This is also reflected in the spectral curve of the arterial Doppler, which under normal conditions shows a triphasic pattern, but with smaller amplitudes. The method for PAD-LL evaluation by Doppler ultrasound is an easily accessible, relatively inexpensive, and completely non-invasive method compared to other radiological methods. Doppler ultrasound provides information about the morphology of blood vessels and blood flow, whereas pulsed Doppler velocity is used to determine the intensity of arterial stenosis. Flow velocity is increased in stenotic areas as blood needs to move faster to maintain the same volume as it passes through the normal lumen to pass through the narrowed lumen [29].
The peak systole progressively increases with narrowing until the flow resistance becomes so high (diameter reduction greater than 80%) that peak systole drops to normal or even subnormal values [30]. Disadvantages of Doppler ultrasound include user-dependent results and difficulties in distinguishing high-grade stenosis, evaluating sequential layout lesions, and capturing images of the vascular lumen with calcified plaques [29]. In the case of inflammation or increased vascularization, IRT revealed an increase in the temperature of the segment or region of the body under study, while in the case of PAD-LL, there was a decrease in temperature due to obstruction of the arterial blood flow. ABI is a simple, non-invasive, and widely accepted diagnostic test that compares blood pressure in the upper and lower limbs [31]. ABI generally ranges from 1.00 to 1.29, and an ABI ≤ 0.90 is used to diagnose PAD-LL in the clinical setting [32, 33]. In symptomatic patients, when compared to arteriography, an ABI ≤ 0.90 has a sensitivity of approximately 95% for detecting PAD and a specificity of almost 100% for proving the absence of PAD-LL [34]. The use of IRT as a diagnostic tool is not new. However, despite the optimistic results of several studies, it should be used as a complement to the gold standard methods for the diagnosis of PAD-LL. Knowledge of thermoregulation, anatomy, physiology, morphology, and pathophysiological processes is important to avoid inaccurate diagnoses [35]. More research and follow-up studies are needed to create databases of clinical measures and determine their feasibility for diagnosing PAD-LL [35]. Considering the advantages of IRT as a non-invasive, non-irradiating, and low-cost test and the high resolution of existing thermal cameras, further studies should evaluate the feasibility of IRT as a complementary diagnostic tool or screening test for PAD-LL.
In conclusion, in the current study, a portable IRT device showed high sensitivity and specificity as a screening tool for lower limb arterial disease compared to arterial Doppler ultrasonography. The method was found to be limited in diagnosing patients with PAD above their knees (i.e., suprapopliteal PAD). Our results suggest that for values ≤ 0.90, ABI can be a valuable predictor for PAD-LL when adequate standardization is followed, and the ABI is adequate for discarding PAD-LL. Current or previous smoking, BMI, and diabetes mellitus were statistically significant risk factors for PAD-LL. The results presented here suggest that IRT can be an efficient and low-cost method for screening PAD-LL, particularly for infrapopliteal PAD-LL manifesting below the knees. More high-powered studies are needed to establish the validity of this technique and, in addition, to define the best methodology for its use.